What is meningococcal disease?
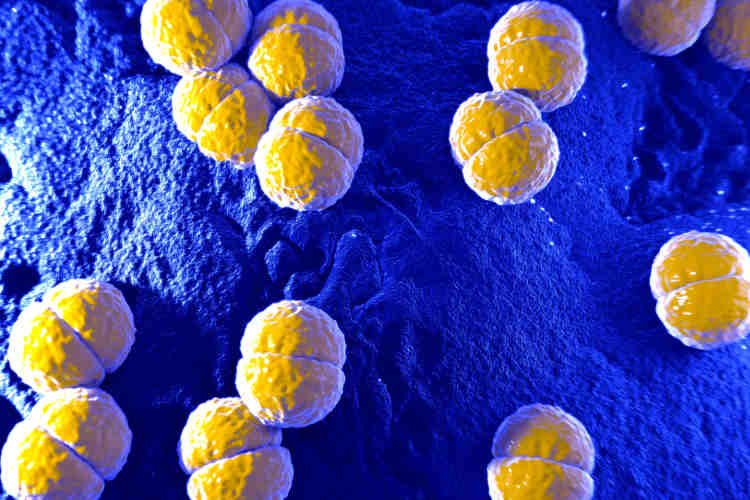
Meningococcal disease is an infection caused by a type of bacterium known as meningococcus, or Neisseria meningitides. It is a rare but serious illness, occurring mostly in winter and early spring in Australia.
The main forms of invasive meningococcal disease include:
- Meningitis, where the infection involves the meninges — the covering of the brain and spinal cord.
- Meningococcal septicaemia, where the bacteria invade the bloodstream causing blood poisoning.
- A combination of meningitis and septicaemia.
The main treatment is with antibiotics, which need to be given as soon as possible to avoid complications from the infection.
Symptoms and signs
People with meningococcal disease are usually very unwell.
Symptoms and signs of meningococcal septicaemia may include:
- High fever.
- Lethargy, drowsiness, irritability or confusion.
- Vomiting and/or diarrhoea.
- Cold hands and feet.
- Pain in the joints or muscles.
- A rash, which may start as very small red or purple spots then enlarge to look like bruises.
The rash associated with meningococcal disease doesn’t go away or disappear when you gently apply pressure to the skin (for example pressing it with your finger or the side of a clear drinking glass that you can see through).
People with meningococcal meningitis may have the following symptoms:
- Fever that comes on suddenly.
- Severe headache.
- Dislike of bright lights (photophobia).
- Neck stiffness.
- Cold hands and feet.
- Lethargy, drowsiness, irritability or confusion.
- Vomiting.
- Seizures (fits).
- Pain in the joints and muscles.
In young babies the signs of meningococcal disease may differ from those in older children and adults, and may include:
- Fever.
- Drowsiness.
- Floppiness.
- Irritability.
- Dislike of being handled.
- A high-pitched moaning cry.
- Disinterest in or refusing to feed.
- Vomiting and/or diarrhoea.
- A rash of red-purple spots or bruises.
- Pale, blotchy skin.
- A bulging fontanelle (soft spot on top of the head).
It is important to remember that most of the time not all of these symptoms are present.
Infection with meningococcal disease can develop very quickly, and can be fatal. Anyone with symptoms or signs suggestive of the disease requires medical attention immediately.
Causes
Some people carry the meningococcus bacteria in their noses or throats and yet remain well — these people are known as carriers.
Carriers can spread the bacteria to other people, usually through fine droplets spread by coughing or sneezing but also through direct contact. Among people who catch the infection, symptoms usually start to develop within 3-4 days of being infected.
Risk factors
Anyone can develop meningococcal disease, but it is more common in the following groups.
- Children under 2 years of age.
- Healthy adolescents aged 15-19 years.
- Young adults aged 20-24 years living in close quarters (for example, student accommodation).
- Young adults aged 20-24 years who smoke.
- Indigenous Australian children and adolescents.
- People with problems with their immune systems, including people without a functioning spleen.
Smoking, passive exposure to cigarette smoke and intimate kissing with multiple partners can also put you at higher risk.
Diagnosis and tests
If you are concerned that you or someone you are with may have meningococcal disease, you should call 000 for an ambulance or go straight to the nearest hospital emergency department.
A doctor will ask about your symptoms, how long you have had them, and whether you know anyone else who has been sick with similar symptoms. They will perform a physical examination, including measuring your temperature, pulse and blood pressure, and looking for any evidence of a rash.
Tests that are usually done when meningococcal disease is suspected include the following.
- Blood cultures, to test for the presence of Neisseria meningitides in the blood.
- Lumbar puncture, where a sample of cerebrospinal fluid (CSF) — the fluid that surrounds the brain and spinal cord — is taken and tested for evidence of meningococcal infection.
- Head CT or MRI to check for evidence of swelling or inflammation around the brain.
Treatment for meningococcal disease
People with meningococcal disease need treatment in hospital. They will need to be monitored closely and given fluids and medicines directly into their bloodstream (via a tube into a vein).
Antibiotics are needed to treat the infection. Because people with meningococcal disease are often very unwell, the antibiotics are given via a drip into a vein.
With early diagnosis and treatment, most people make a full recovery.
Some people will suffer long-term complications following a meningococcal infection, such as:
- hearing impairment (deafness) or ringing in the ears;
- double vision;
- aching joints or limb deformities;
- scarring of the skin; or
- brain damage and learning difficulties.
Vaccination
The best way to protect yourself and your children from meningococcal disease is to get vaccinated. Of the several different strains (serogroups) of meningococcal disease, those that most commonly cause disease in Australia are groups A, B, C, W, and Y. Vaccines are available in Australia against these strains.
MenACWY vaccines (Menactra, Menveo, Nimenrix) offer protection against 4 strains (A, C, W and Y) and a separate MenB vaccine (Bexsero) can protect against meningococcal B. Anyone who wants to protect themselves against meningococcal disease is recommended to have these vaccines.
Vaccination is strongly recommended for infants, children, adolescents and young adults; special risk groups, including indigenous Australians; people with certain medical conditions that increase their risk; some laboratory workers; travellers; and young adults who smoke or live in close quarters.
MenACWY is also recommended as a travel vaccination for people travelling overseas to areas where meningococcal disease is more common or when travelling to mass gatherings, such as the Hajj.
Getting vaccinated
Meningococcal vaccines currently available for free as part of the National Immunisation Program in Australia include:
- MenACWY at 12 months of age for all children.
- MenACWY at 14-16 years through school programs for all children. A catch-up dose is available for 15-19 year olds who miss out on having it at school.
- MenB for indigenous children only, at 2 months, 4 months, 6 months (for indigenous children with specified medical risk conditions), and 12 months.
The National Immunisation Program does not currently cover the MenB vaccine for non-indigenous children. However, the vaccine is available on private prescription and there are state and territory-based programmes for meningococcal vaccines. For example, MenB is available for free for children and young people living in South Australia, funded by the South Australian State Government.
Booster doses are needed for some people – talk to your doctor about immunisation and whether booster shots will be needed.
Remember, no vaccine is able to offer 100 per cent protection against meningococcal disease. So, even if you’ve been immunised, it’s important to seek immediate medical attention if you develop any symptoms of meningococcal disease.
Meningococcal vaccination side effects
Possible side effects associated with meningococcal vaccination include:
- redness and soreness at the injection site;
- fever;
- irritability or drowsiness in young children;
- decreased appetite; and
- headaches.
Fever is a common side effect associated with meningococcal B vaccine, especially when used in children aged 2 to 12 months. It is recommended that paracetamol is given with meningococcal B vaccine to prevent or reduce fever.
Antibiotics to prevent infection
Anyone who has been in close contact with someone with meningococcal disease, such as members of the same household, will be given antibiotics to prevent infection.
But it’s important to be aware that even when contacts take antibiotics, infection is still possible, so immediate medical help is needed if they develop any symptoms.
Where to get help
Remember, call 000 for an ambulance for any medical emergency. If you are very unwell or have symptoms of meningococcal disease, call 000 or go to the local hospital emergency department.
See your GP (general practitioner) or go to your local community health clinic for vaccination against meningococcal disease.