Cellulitis is a bacterial infection of the skin, most commonly caused by Staphylococcus aureus (staph) and Group A beta-haemolytic streptococcus (also known as Streptococcus pyogenes) – two types of bacteria. These bugs may live on your skin surface, but sometimes they can enter into the deeper layers when skin is broken, such as by a cut or a scratch, or even through apparently undamaged skin. The infection can spread quickly and become very dangerous and so cellulitis requires treatment with antibiotics.
Cellulitis can affect any part of the body, but in adults it commonly affects the skin of the lower legs. In children, cellulitis commonly affects the skin around the eye. This situation is potentially sight threatening and needs to be seen by a doctor promptly.
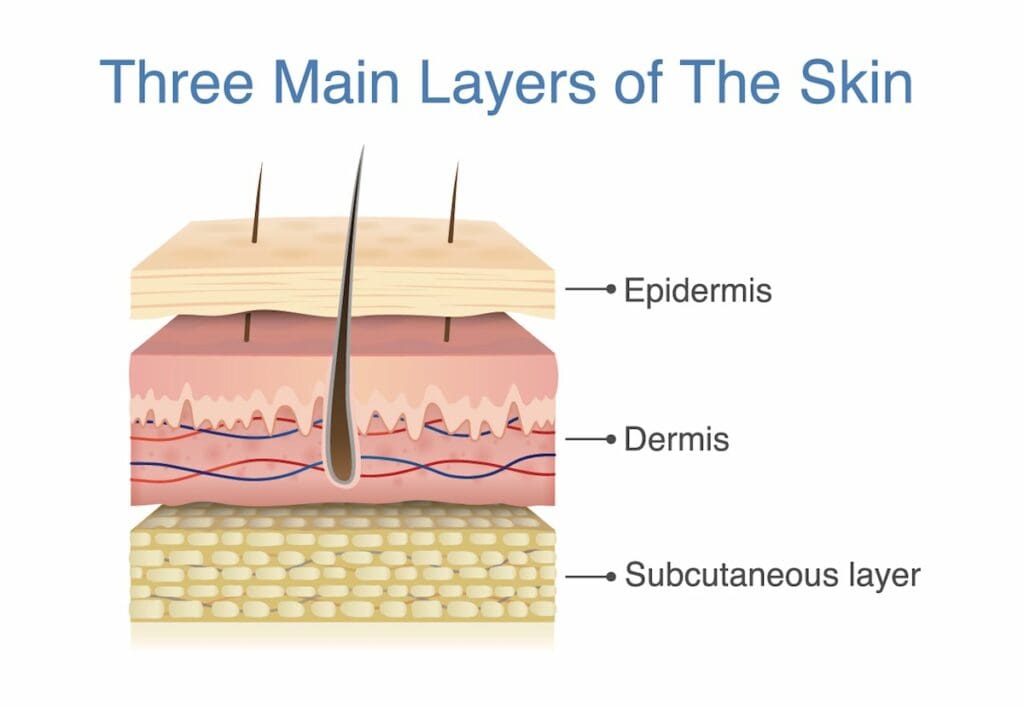
Cellulitis is an infection of 2 of the skin’s 3 layers – the middle (dermis) and the deep layers (subcutaneous tissue).
Erysipelas is a subtype of cellulitis that involves the upper dermis (upper middle layer) and the epidermis (upper layer of skin). It often involves the skin on the face, but also commonly affects the legs. It is more common in young children and older adults. The treatment for cellulitis and erysipelas is the same.
Symptoms
If cellulitis is not treated promptly it may become life-threatening, so if you have symptoms of cellulitis, seek medical help immediately.
Cellulitis typically starts as a red and painful patch of skin. It is generally warm to touch and the area may feel swollen and tighter than the surrounding skin. This affected skin area may get larger.
You may get enlarged glands (lymph nodes) near the area of cellulitis. There also may be an obvious entry point to the deeper layers of skin such as a cut or scratch. Sometimes there is leaking of pus or clear or yellow fluid.
Symptoms such as fevers, shakes and chills indicate that the infection is severe, or worsening quickly, and you must seek emergency medical help immediately.
What causes cellulitis?
As mentioned, the cause of cellulitis is a bacterial infection of the skin and underlying tissues. As well as Streptococcus pyogenes, Staphylococcus aureus (including methicillin-resistant Staphylococcus aureus – MRSA) and other bacteria can be a cause of cellulitis.
Common areas of the skin that become infected are:
- cuts, scratches, insect or animal bites, burns or grazes;
- surgical wounds;
- areas where a foreign object is in the skin, such as a splinter or glass;
- areas where there are already skin problems such as acne, eczema or psoriasis.
Sometimes the exact site of entry can not be found and the bacteria appear to have entered through normal unbroken skin.
Risk factors
Cellulitis can affect anybody, but you are at higher risk if you:
- smoke;
- have diabetes;
- have had cellulitis before;
- have a wound, cut or ulcer;
- have poor circulation;
- have lymphoedema – accumulation of lymphatic fluid in the body due to a blockage, leading to swelling; or
- have athlete’s foot – a fungal infection commonly found between the toes.
Complications
Cellulitis can cause serious harm if left untreated. Sometimes cellulitis can cause an abscess (a collection of pus beneath the surface of the skin).
Cellulitis can cause problems in the surrounding area such as permanent damage to the skin and gangrene (tissue death). If the infection damages the veins and the lymphatic vessels draining the area, such as in people who have repeated episodes of cellulitis in the same area, there may be permanent swelling of the affected tissue.
If cellulitis is not treated with antibiotics, the infection can spread to the bloodstream and lead to sepsis. Sepsis is an extremely dangerous infection of the blood which can lead to death.
Tests and diagnosis
Cellulitis is usually diagnosed based on the appearance of the skin and other signs or symptoms you may have. Usually, oral antibiotics (tablets or capsules) will be prescribed to be started straight away. Your doctor may take a swab of the area to send to the laboratory to see what type of bacteria is causing the cellulitis. This is mainly useful when the cellulitis has pus or there is a wound or ulcer associated with the cellulitis.
Blood tests are not done routinely, but the doctor may order a full blood count or blood culture. Imaging such as an X-ray, ultrasound or CT scan may be done to rule out other diagnoses.
Treatment
Your doctor may use a pen to mark the area of redness so they can see if it is spreading or staying the same size. Antibiotics are required to treat the infection.
If you only have a limited area of pain and redness, without any signs of being systemically unwell, then oral antibiotics (antibiotics taken by mouth) for at least 5 days is usually enough to clear the infection. It is important to finish the course of antibiotics, even if you start to feel better after a few days.
If you are unwell with fevers, chills or shakes the doctor may use intravenous (into the vein through a drip) antibiotic therapy. This allows a stronger dose and faster absorption. Once you begin to feel better you can be switched to oral antibiotics. The total course of treatment for both intravenous and oral antibiotics will be between 5 and 10 days.
Type of antibiotic
The doctor will prescribe antibiotics based on an educated guess of which type of bacteria is most likely to be causing the infection.
Group A beta-haemolytic streptococcus is suspected when there is no pus, the cellulitis is rapidly spreading and it is recurrent or spontaneous. The antibiotics usually used in this situation are phenoxymethylpenicillin orally or benzylpenicillin intravenously.
Staphylococcus aureus is suspected when there is broken skin, pus or an associated ulcer. The antibiotics recommended are dicloxacillin or flucloxacillin orally, or in severe cases flucloxacillin intravenously. If MRSA is likely or suspected, the antibiotics given may differ.
People who are allergic to penicillin may be given other antibiotics.
If a swab has been sent to the laboratory, it may later confirm which type of bacteria is responsible for the infection. If the laboratory identify the bacteria causing the cellulitis, they can test which antibiotics are effective at treating it (this is called antibiotic sensitivities).
MRSA and cellulitis
Methicillin-resistant Staphylococcus aureus (known as MRSA) is a type of Staphylococcus bacteria that’s become resistant to many of the antibiotics normally used to treat it. MRSA can cause purulent cellulitis (cellulitis with pus).
MRSA is transmitted by contact with a person who carries it on their skin, contact with contaminated wounds or bandages, contact with contaminated objects or inhalation of droplets from a person who carries MRSA in their nasal (nose) passages.
If MRSA is suspected or is likely as the cause of cellulitis, initial treatment will be with antibiotics, which may be changed if antibiotic sensitivities are established after the results from a swab.
Surgery
Surgery is generally not needed for cellulitis. Rarely, dead tissue may need to be surgically removed to improve healing.
Abscesses can develop alongside cellulitis and these require an incision and drainage (cut into the skin to manually remove the pus) usually under local anaesthetic. Abscesses usually also require antibiotics but this can depend on individual circumstances.
Is cellulitis contagious?
Cellulitis isn’t contagious – it doesn’t usually spread from person to person. It is an infection of the deeper layers of skin, most often caused by bacteria that live on the surface of your skin.
What can you do at home?
As well as taking the antibiotics prescribed by your doctor, there are some things you can do at home to help cellulitis.
- Get plenty of rest to give your body time to heal.
- If there is a large area of swelling, raising up the infected area will help to reduce swelling and pain.
- Over-the-counter painkillers such as paracetamol and ibuprofen (discuss with your doctor) can be used to reduce pain.
- Make sure to keep the wound area dry and clean whilst it is healing. If the wound dressing becomes wet, it will need to be changed.
What to expect
The redness can worsen up to 48 hours after the correct antibiotic therapy is started, but most people with cellulitis who take their antibiotics have their symptoms improve in a couple of days. You may need a follow-up appointment with your general practitioner to check that the infection is improving. If the redness keeps getting bigger or you begin to feel more sick with fevers, go to your doctor or the emergency department immediately. Cellulitis around the eye will need to be closely monitored by a doctor.
Prevention
Recurrent cellulitis is common in people with risk factors, such as lymphoedema, eczema or a weakened immune system. You may benefit from controlling your risk factors such as keeping your skin hydrated, caring for ulcers or wounds correctly and treating conditions such as psoriasis, eczema and athlete’s foot. Preventative antibiotics may also be useful in avoiding recurrent cellulitis.




