Neuropathic pain (nerve pain) affects about one in every 20 people in Australia. It is caused by damage to nerves that feel pain, touch and temperature. The pain has been described as a burning, shooting or crawling sensation or like electric shocks, and there are often other feelings, such as numbness or pins and needles that accompany the neuropathic pain.
There are several specific types of neuropathic pain, including trigeminal neuralgia, painful diabetic neuropathy and postherpetic neuralgia (a complication of shingles). Neuropathic pain is often severe, ongoing (chronic) and can be difficult to treat.
What happens when you have nerve pain?
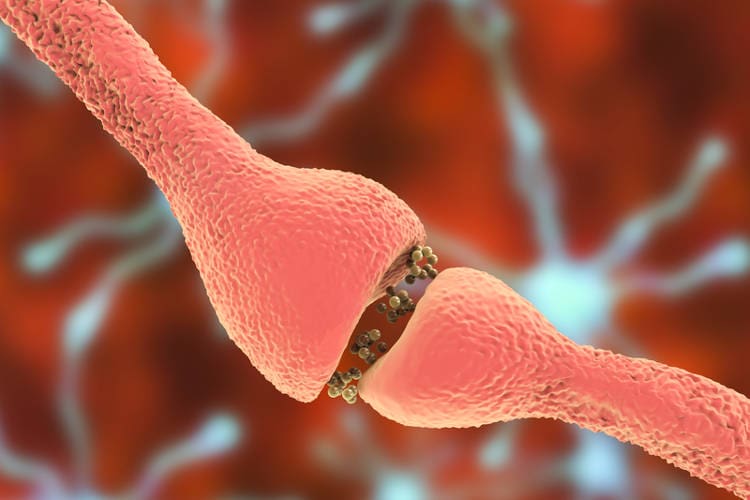
Usually, pain is felt when your nerve endings sense that something is wrong with your body and send pain signals to your spinal cord and brain. Neuropathic pain occurs when the nerves themselves are damaged by disease or injury, causing them to misfire and send pain signals to the brain.
Symptoms of neuropathic pain
Neuropathic pain is usually described as shooting, stabbing or burning. Sometimes it feels like an electrical shock, and is often worse at night than during the day. The pain may be constant or it may come and go. It may be accompanied by tingling sensations (such as pins and needles), itching or numbness.
People with neuropathic pain are often extremely sensitive to normal painful stimuli – that is, they feel pain more intensely than other people. They may also have increased sensitivity to touch or cold, and may perceive non-painful stimuli, such as light touch or gentle brushing of the skin, as painful.
What causes neuropathic pain?
Neuropathic pain is caused by damage to the somatosensory nervous system – the part of the nervous system that feels pain and other sensations such as touch and temperature. The damage can be due to illness or injury, and may affect the brain, spinal cord, or the nerves in the rest of the body (the nerves in your face, arms, legs and torso).
While doctors are sometimes unable to pinpoint the exact cause of neuropathic pain, there are several known causes, including:
- injury;
- spinal cord damage;
- diabetes;
- nerve compression (trapped nerve), such as in carpal tunnel syndrome or sciatica;
- nerve invasion by a tumour;
- infections such as shingles and HIV/AIDS;
- multiple sclerosis;
- stroke;
- some types of chemotherapy; and
- vitamin B12 or thiamine (vitamin B1) deficiency.
Specific types of neuropathic pain
Some examples of neuropathic pain include the following.
Painful diabetic neuropathy
Having diabetes and high blood sugar levels can damage your nerves, especially those in the legs and feet. This condition – diabetic neuropathy – can cause pain as well as numbness and tingling.
Trigeminal neuralgia
Trigeminal neuralgia is a disorder of the trigeminal nerve — the nerve that supplies sensation to the face and controls some of the muscles involved in chewing. People with trigeminal neuralgia have episodes of severe facial pain that last from a couple of seconds to several minutes.
Post-herpetic neuralgia
About one in every 5 people with shingles (a painful rash also known as herpes zoster) develops post-herpetic neuralgia — ongoing pain in the area that was affected by the rash. It occurs when the shingles virus damages the underlying nerves, and the resulting pain can last for months or years.
Phantom limb pain
This condition affects people who have had an arm or leg amputated, causing pain or discomfort in the area of the now-missing limb. The exact cause of phantom limb pain is not known, but it is thought to be due to changes in both the nerves of the affected limb and the central nervous system (brain and spinal cord) following amputation.
How is neuropathic pain diagnosed?
If your doctor suspects you may have neuropathic pain, he or she will ask about your pain and any other sensations you experience, such as pins and needles or numbness. Your doctor will also want to know about any events or illnesses that may have caused it.
Your doctor will perform a physical examination, testing the nerves in the affected area. They may touch the skin in the the affected area with cotton wool, toothpicks or warm or cool objects as part of the examination.
If your symptoms and physical examination suggest you have neuropathic pain your doctor can prescribe specific treatment for this type of pain.
To make a definite diagnosis of neuropathic pain, the underlying cause of the pain needs to be found. Your doctor may recommend tests including:
- blood tests;
- nerve conduction studies (to measure how quickly your nerves can carry electrical signals); or
- an MRI scan.
Sometimes a biopsy (tissue sample) can help with diagnosis. A skin biopsy (looking for a reduced density of nerve fibres in the skin) or a nerve biopsy (looking for abnormalities in the nerve fibres) may be recommended.
Complications
Having ongoing pain can have a significant effect on your entire life. It can cause problems sleeping, affect your ability to work and attend social events, and even lead to depression and anxiety.
Adequately treating neuropathic pain and learning coping strategies to manage pain are very important to make sure that you maintain a good quality of life.
Who treats neuropathic pain?
Your general practitioner (GP) will probably be the first person you see about your pain. GPs can diagnose and treat neuropathic pain, but some people may benefit from a referral to a pain specialist or pain clinic.
Healthcare professionals who can help in the treatment of pain include occupational therapists, psychologists, nurses and physiotherapists.
Treatment
Neuropathic pain is different from other types of pain, so different medicines are needed to treat it. There are several medicines available in Australia that can be used to help relieve this type of pain. Unfortunately, neuropathic pain is often not completely controlled by medicines, so other treatments are also usually recommended to help you manage the pain and improve your quality of life. These include psychological therapy, meditation and physical activity. Treatment of the underlying cause of the pain is also important.
Medicines
The medicines that are generally most effective in treating neuropathic pain are:
- antidepressant medicines; and
- anticonvulsant medicines (the same medicines that are used to control seizures in people with epilepsy).
These medicines can be used for all causes of neuropathic pain, but some medicines are preferred over others for specific types of neuropathic pain.
When deciding which medicine to prescribe, your doctor will consider:
- the cause of your pain;
- your overall health;
- other medicines you are taking;
- the cost of the medicine; and
- side effects.
Medicines for neuropathic pain are usually started at a low dose, and gradually increased if needed – it may take a few weeks for the medicine to have an effect. Your doctor will closely monitor your response to the medication and any side effects you are experiencing.
Antidepressant medicines
Tricyclic antidepressants (tricyclics) are a type of antidepressant that has been found to relieve neuropathic pain in many people. These medicines have a pain-relieving effect that is separate from their antidepressant effect, and may be especially useful in relieving constant, burning pain.
Amitriptyline is the most commonly used tricyclic antidepressant for treating neuropathic pain. Doxepin or nortriptyline may be used as alternatives. Side effects of tricyclics can include constipation, dizziness, tiredness and dry mouth. However, when used in low doses, as recommended for neuropathic pain, side effects are less problematic.
Another class of antidepressant medicine – the serotonin and noradrenaline reuptake inhibitors (SNRIs) – can also relieve neuropathic pain. Duloxetine (examples of brand names include Andepra and Cymbalta) is the SNRI usually prescribed to treat neuropathic pain such as painful diabetic peripheral neuropathy. Venlafaxine is another SNRI that can be used by specialists for treating neuropathic pain. Side effects of SNRIs can include nausea, diarrhoea, reduced appetite, headaches and sexual dysfunction (including reduced libido and difficulty having an orgasm).
Anticonvulsant medicines
Anticonvulsant medicines can also be effective in treating neuropathic pain, and work by slowing or blocking uncontrolled pain signals. Anticonvulsants may be better than tricyclics for treating sharp, shooting neuropathic pain.
Gabapentin (e.g. Gantin, Neurontin, Nupentin, Pendine) and pregabalin (e.g. Lypralin, Lyrica, Lyzalon) are anticonvulsant medicines that can relieve neuropathic pain. They have been found to be useful in treating painful diabetic neuropathy and post-herpetic neuralgia. Side effects of these medicines can include tiredness, dizziness and weight gain.
Carbamazepine (e.g. Tegretol, Teril) – another type of anticonvulsant medicine – is usually the first choice of medicine for treating trigeminal neuralgia.
Other medicines
If antidepressants and anticonvulsants do not relieve your pain, you doctor may suggest trying another type of medicine, which may need to be prescribed by a specialist pain physician.
Local anaesthetics (e.g. lidocaine (lignocaine) cream or skin patches) and capsaicin cream (which contains a substance extracted from red chilli peppers) may be effective in treating some types of neuropathic pain, such as post-herpetic neuralgia. These medicines, which are applied directly to the skin, can have side effects such as local pain, redness and irritation.
Pain relievers such as tramadol (e.g. Tramal, Tramedo, Zydol) may be prescribed short-term in some cases where the pain is severe. Side effects of tramadol include dizziness, dry mouth, tiredness, nausea and constipation.
Strong opioid pain relievers (such as morphine) are not usually recommended because they are not very effective in the long-term and there are safety concerns with these medicines. Simple pain relievers such as paracetamol and nonsteroidal anti-inflammatory drugs (NSAIDs) are generally not effective for neuropathic pain.
A combination of several medicines may be effective for some people, especially those who have a partial response to one or more medicines. More research is needed to work out how effective and safe combination treatments for neuropathic pain may be.
Other treatments
Other treatments that may help to control neuropathic pain include the following.
- Relaxation techniques and meditation, which are used to reduce any muscle tension that is contributing to pain.
- Psychological treatments, such as cognitive behavioural therapy (CBT), which can help you gain a sense of control over pain and reduce distress. CBT involves identifying and challenging negative thinking patterns and developing different ways of thinking and responding.
- Transcutaneous electrical nerve stimulation (TENS), which uses mild electrical currents (from electrodes that are taped to the skin near the site of the pain) to block the transmission of pain sensations to your brain. TENS machines can be purchased from pharmacies, and TENS can be done at home.
- Percutaneous electrical nerve stimulation (PENS) is similar to TENS, but the electrical currents are applied via a needle electrode that is inserted under the skin. This treatment may be recommended by a pain specialist for people with neuropathic pain that is difficult to treat.
Some people have tried acupuncture to help relieve neuropathic pain, but there is currently no evidence from clinical trials showing that acupuncture is effective for this type of pain. Several trials are ongoing.
Pain specialists may also recommend more invasive treatment options if other treatments have not been effective. These may include injections, nerve blocks or surgery. Your doctor can talk you through the options, their pros and cons, and whether they may be suitable for you.
Self-care
Many people find that being as physically active as possible helps them cope with neuropathic pain. Physical activity can help reduce stress and improve fitness. Gentle stretching and yoga can be good options. Make sure you pace yourself and plan your activities carefully so that you are not overdoing it.
Getting enough sleep and eating a healthy diet are also important. A healthy diet tends to reduce inflammation in the body and this may be helpful in neuropathic pain.
What’s the outlook for neuropathic pain?
While neuropathic pain can be ongoing for many people, there are treatments available to help relieve and manage the pain. Treating the underlying cause of the pain as well as the pain itself is important, as is seeing a pain specialist sooner rather than later.
Clinical trials investigating neuropathic pain will help better our understanding of this type of pain and develop new and innovative treatments.
Support groups for neuropathic pain
Living with neuropathic pain is often very challenging. Support groups can give you an opportunity to meet others who are going through a similar experience. Understanding from others can help you feel less isolated, and you may also be able to exchange tips on coping with pain and ways to manage. Search the internet or ask your doctor about neuropathic pain support groups.