What is retinal detachment?
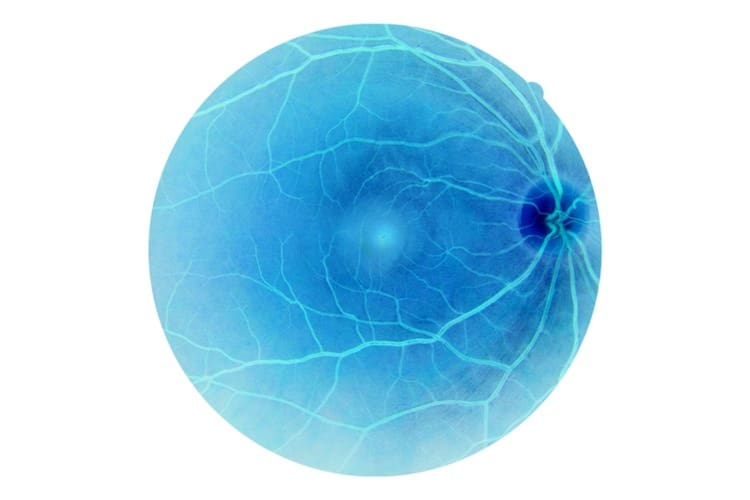
Retinal detachment occurs when the retina, the light-sensitive nerve tissue lining the inside of the eye, becomes separated from where it is normally attached at the back of the eye. When this happens, the retina stops functioning, causing loss of vision. The retina is responsible for converting light into nerve impulses that are then sent along the optic nerve to the brain.
Retinal detachment is a medical emergency. If not treated properly, it can lead to permanent blindness in the affected eye when the retina becomes permanently detached.
Although retinal detachment is rare, affecting 1 in 10,000 Australians every year, the consequences can be catastrophic loss of sight, so if you have symptoms of retinal detachment, such as sudden onset of floaters or flashes, you should contact an eye specialist (ophthalmologist) or your doctor immediately. This could save your sight.
Retinal detachment may start with tears or holes in the retina – if these aren’t treated they may lead to retinal detachment.
Symptoms
Symptoms of retinal detachment may include:
- Sudden onset of, or a sudden increase in, ‘floaters’ (dark moving specks or ‘cobwebs’) and flashes (momentary flashes of light like a camera flash or lightning bolt) that appear in your vision.
- Sudden deterioration in, or loss of, vision. This is commonly described as a ‘curtain’ or ‘shadow’ appearing across the field of vision, often starting on one side and moving towards the centre.
- Blurred vision.
- Loss of peripheral vision (vision at the sides).
If you have sudden onset of these symptoms you should visit a doctor or an ophthalmologist immediately.
Flashes and floaters also occur as normal age-related changes to the eye, and are present in two-thirds of over 70-year-olds. They are often associated with posterior vitreous detachment (PVD), a condition causing some tugging on the retina. PVD requires no treatment, but is associated with increased risk of retinal detachment. It can be hard to determine if these symptoms are due to PVD or are warning signs of retinal detachment so all flashes and floaters should have same day assessment by an eye specialist.
A detached retina causes no pain when it separates.
Risk factors
The risk of developing retinal detachment is higher in people with:
- advancing age;
- short-sightedness;
- a previous eye injury;
- previous cataract surgery;
- a history of retinal detachment in the other eye; or
- a family history of retinal detachment.
What causes a detached retina?
There are 3 types of retinal detachment, each caused by different mechanisms:
- Rhegmatogenous: this is when a hole or tear develops in the retina, allowing fluid from the vitreous (the jelly that fills the middle of the eye) to pass through the tear and build up between the retina and the underlying tissue, thus separating the retina from the underlying tissue by lifting it off; this is the most common type of retinal detachment.
- Tractional: scar tissue pulls the retina away from its attachment. This can be caused by infection, trauma and haemorrhage.
- Exudative: leakage of fluid underneath the retina causes separation, and may be due to one of several causes, including leaky blood vessels or inflammation; this is the least common type of retinal detachment.

Diagnosis of detached retina
Your doctor will usually refer you to an ophthalmologist (eye specialist) on the same day. They will want to know if you are experiencing changes in one or both eyes, and whether your vision is affected. The ophthalmologist will examine your eyes and may use some eyedrops to dilate your pupils.
Sometimes ultrasound is necessary to help with diagnosis.
Treatment
If you have symptoms of retinal detachment, you must seek medical attention immediately. If treatment is delayed, there can be permanent loss of vision.
Treatment of retinal holes and tears
Small holes or tears which occur before the retina has detached, will need to be treated, so they don’t progress to be a detached retina. These may be treated with:
- laser surgery – this burns around the tear, creating scar tissue that helps the retina to stay attached to the tissue underneath.
- freezing (cryopexy/cryotherapy) – a very cold instrument is touched onto your eye where the tear is. This also causes scar tissue to help the retina stay attached.
Treatment of a detached retina
If the retina has detached, surgery is required to re-attach it and to repair any holes or tears.
There are several different surgical options for the treatment of retinal detachment, and the choice of procedure will depend on your individual circumstances.
Possible complications of surgery
There are risks with any type of surgery, including infection, bleeding and risks associated with the anaesthetic. Your doctor will discuss these with you before any procedure.
Side effects associated with some procedures used to treat retinal detachment can include vision problems (such as short-sightedness) and an increased risk of developing cataracts.
For a few weeks after eye surgery for retinal detachment, your eye may feel uncomfortable and watery. Make sure to follow your doctor’s instructions on caring for your eyes after surgery.
In a small number of people the retina re-detaches and a second operation is needed.
Will I get my vision back after retinal detachment?
The amount of vision recovered after surgery will depend on how much of your retina has detached. Overall, about 95 per cent of cases of retinal detachment will be able to be repaired, with at least some vision preserved. The outcome is worse if the macula (central vision) is involved. The quicker you can see an eye specialist, the better the results of surgery may be.
It may take a few months for your vision to improve and some people won’t be able to see as well as they did previously.
Remember, if you’ve had a retinal detachment already, you are at increased risk of having one in the other eye, so be sure not to delay if you have any symptoms.