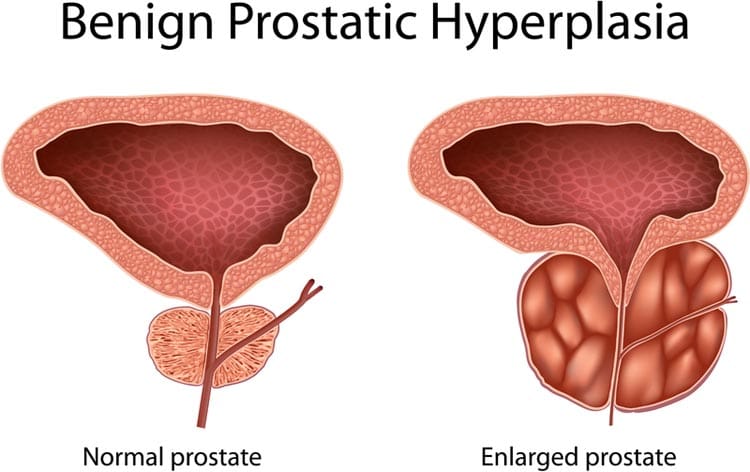
Enlargement of the prostate gland – a small, walnut-sized organ located under the bladder and near the rectum, or back passage, in men – is a common condition.
The prostate surrounds the tube – called the urethra – that carries urine from the bladder out through the penis. The prostate continues to grow as men age, and from around the age of 50, an enlarged prostate may put pressure on the urethra and the base of the bladder. The increased pressure from the prostate makes it harder for urine to pass through the urethra when urinating. An enlarged prostate is not usually life-threatening but the troublesome symptoms can significantly affect men’s enjoyment of life.
| What is the prostate? | |
|---|---|
 |
|
| The prostate is a small gland that sits underneath the bladder and surrounds the top part of the urethra.
The prostate makes fluid secretions that support and nourish sperm. This fluid is squeezed into the urethra during ejaculation. |
|
What are the symptoms of prostate enlargement?
Not every man with an enlarged prostate has symptoms. But when symptoms do occur, they are related to the prostate obstructing the flow of urine through the urethra. This can lead to problems such as:
- Difficulty in starting or stopping urination;
- Dribbling of urine after urination has stopped (incontinence);
- A weak urine stream;
- A frequent and urgent need to urinate, particularly at night;
- Blood in the urine;
- Pain in the area between the scrotum and the anus; and
- A feeling that the bladder is not empty even after urinating.
Although these symptoms are usually due to an enlarged prostate, they may also be caused by other serious conditions (such as cancer of the prostate or bladder). So men should always see a doctor if they notice changes in the how they urinate, or how often.
Complications of prostate enlargement
Left untreated, an enlarged prostate may lead to a number of complications, including:
- Pain in the lower abdomen due to the urethra becoming too narrow. Urine cannot flow through the urethra normally, which leads to a painful build-up of urine in the bladder;
- Bladder infections due to stale urine sitting in the bladder which becomes infected with bacteria;
- Bladder stones – small, hard, gritty lumps that form in the bladder, due to the build-up of stale urine in the bladder. The stones don’t usually cause any problems when they are in the bladder, but if they pass into the urethra, they may become stuck and cause sudden severe pain;
- Interrupted sleep because of the need to get up several times during the night to urinate;
- A lower quality of life because of the inconvenience and embarrassment of problems with urination; or
- Serious kidney problems if the flow of urine out of the bladder becomes blocked and causes a build-up of pressure all the way back to the kidneys.
What causes prostate enlargement?
The causes of prostate enlargement are not yet fully understood but are thought to be related to the male sex hormone (testosterone) which controls the growth of the prostate. The prostate is initially quite small, but as men age, testosterone ‘feeds’ the prostate and it starts to get bigger. From birth to around the early teenage years, the prostate increases in size by around 8 times. It doubles again in size from around the early 20s through to 50 years of age, and then doubles again by around the age of 80. With such large increases in size, it’s easy to see why the prostate can begin to squeeze the urethra and make it difficult to urinate.
There may also be a genetic link to prostate enlargement, because the sons of men with an enlarged prostate are more likely to develop prostate disease.
How common is prostate enlargement?
Prostate enlargement is the most common condition affecting the prostate. In fact, almost all Australian men will experience urinary problems due to an enlarged prostate at some point in their lives. Prostate enlargement also goes by several other names, including the term ‘BPH’, which is short for benign prostatic hyperplasia, or benign prostatic hypertrophy. The word ‘benign’ means that the enlargement is not due to cancer, and ‘hyperplasia’ or ‘hypertrophy’ means that the prostate has grown bigger.
What things can make symptoms worse?
There are a number of things that can aggravate the symptoms of prostate enlargement, including:
- Medicines used to treat depression or Parkinson’s disease;
- Some heart drugs;
- Some cough and cold medicines (like those containing antihistamines); and
- Alcohol.
Should I see a doctor?
You should see a doctor if you notice any of the symptoms listed above. This is particularly important if the symptoms are causing you distress, are accompanied by pain in your abdomen, or if your urine has blood in it. Without medical attention, the condition can worsen and your symptoms may become more troubling.
How is prostate enlargement diagnosed?
Your GP (or a specialist, such as a urologist) will take steps to diagnose the cause of your urinary symptoms. Your doctor may:
- Ask about your personal, medical and family history;
- Ask you to describe your symptoms and how much they interfere with your life;
- Do a physical examination – this will usually include the doctor checking the size, shape and feel of the prostate by placing a lubricated gloved finger into the rectum (back passage);
- Request urine or blood tests – a blood test can check levels of a particular protein. Levels of this protein (called PSA, or prostate specific antigen) can become high due to prostate problems such as an enlarged prostate or prostate cancer; or
- Request an ultrasound scan of your prostate, bladder and kidneys. This may include a scan before and after emptying your bladder to see if significant urine remains after voiding.
Is it prostate enlargement or prostate cancer?
The symptoms of an enlarged prostate can be similar to the symptoms of prostate cancer. So if anything abnormal is found when checking your prostate, your doctor may request a biopsy of your prostate. The biopsy collects a small sample of cells from your prostate which are examined under a microscope to check for the presence of cancer cells.
How is prostate enlargement treated?
There are a number of treatments available for prostate enlargement. The most suitable treatment can depend on how severe the symptoms are:
For mild symptoms
- No treatment may be required if the symptoms are not interfering with your enjoyment of life;
For moderate symptoms
There are medicines that are taken as tablets that can:
- Make it easier to urinate – These medicines are called alpha-blockers and include drugs such as tamsulosin (Flomaxtra), terazosin (Hytrin) or prazosin (Minipress). They generally improve symptoms within several weeks.
- Help to shrink the prostate – These medicines are called 5-alpha reductase inhibitors and include drugs such as finasteride (Proscar) and dutasteride (Avodart). They may take up to 6 months to improve symptoms, and are often combined with an alpha-blocker medicine.
- Herbal medicines such as saw palmetto are commonly used but there is little scientific evidence of benefit.
For severe symptoms
- Surgery may be an option to remove part of the prostate or relieve pressure on the urethra. There are several types of surgery which differ in how they are performed, their recovery times and their possible side effects (see below).
Remember – any medicine or surgical procedure can have side effects. Before making a decision about treatment, you should discuss advantages and disadvantages of each treatment with your doctor to make sure that the choice is a good one for you.
Surgical treatment
There are several types of surgery available to treat prostate enlargement:
- Transurethral resection of the prostate (TURP) – A rigid tube is inserted into the urethra and a metal loop at its end is used to slice off some of the enlarged prostate tissue to reduce pressure on the urethra. TURP is the most common surgical procedure for an enlarged prostate. It is performed under anaesthetic and involves a hospital stay of several days;
- Transurethral incision of the prostate (TUIP) – This procedure also relieves the pressure on the urethra but without removing any of the prostate. It may be used in cases where the enlargement is not severe;
- Open prostatectomy – This is not a common treatment and is usually only done when the prostate is very enlarged. An incision is made in the lower abdomen to remove part of the inside of the prostate; and
- Less invasive treatments – These usually use some form of heat – such as lasers or microwave beams – to reduce the size of the prostate and relieve the pressure on the urethra. Because they are less invasive, they require less time in hospital and have a faster recovery time than some of the other surgical options.
Surgery for an enlarged prostate usually provides significant relief from symptoms and an improvement in quality of life. However, some types of prostate surgery can result in complications which may include bleeding after surgery, infections, problems with sexual function, infertility or leakage of urine. Talk to your doctor or surgeon about the risks associated with surgery.
What can I do to relieve my symptoms?
There are some simple steps you can take that may help relieve your symptoms, including:
- Don’t let your bladder get too full – urinate as soon as the urge arises, and try to relax when urinating. It may help to ‘double void’ – try emptying your bladder again after waiting a moment. Don’t strain or push;
- Reduce your intake of drinks containing caffeine – such as coffee, tea and cola – and alcohol that can irritate the bladder;
- Restrict your intake of fluids before going to bed to reduce the need to get up during the night to urinate;
- Check with your doctor about whether any medicines you are taking might make your symptoms worse and whether there are other alternatives;
- Make sure other health conditions are under control (e.g. diabetes and high blood pressure);
- Do pelvic floor muscle exercises to help stop urine leaking from the bladder (a special nurse or a physiotherapist can teach you the exercises);
- Boost your fibre intake to avoid becoming constipated which can aggravate prostate and bladder symptoms;
- When taking long car trips, make frequent stops to urinate;
- Whenever possible, sit on a hard chair instead of a soft one;
- Lose weight if necessary;
- Quit smoking;
- Be more active; and
- Ask your doctor about natural or herbal supplements that may help relieve symptoms. Herbal extracts may include Saw palmetto, African plum tree or pumpkin seed. But be aware that these products are not as effective as prescription medicines, have not been tested in the same way and may interfere with other medicines you are taking.